Imagine: With eight climbers you’re three quarters on your way climbing the Dufourspitze (4,634m) in the Swiss Alps. Suddenly, a 47-year-old friend of yours slips on polished granite, flipping him upside-down and into freefall. Three meters down the back of his helmet slams into solid rock. You’re more than half a day hiking away from a hut and human civilization and you have only some limited, basic, medical supplies. What would you do?

First Assessment
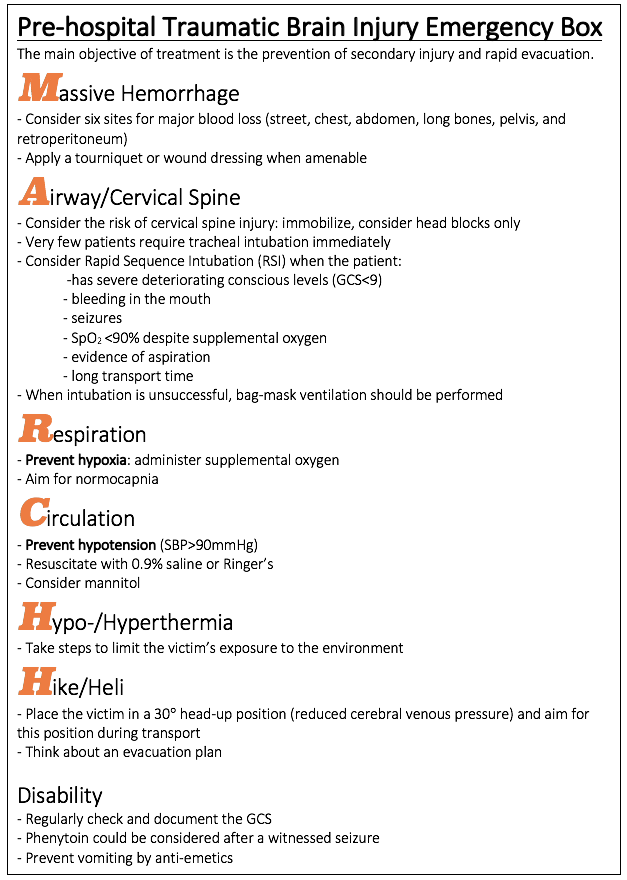
First, check and assess for scene safety (falling rocks, slipping yourself, rope groups, securing on an anchor). Protect yourself and the victim for further harm. Tell the victim who you are, what you’re planning to do, reassure and obtain consent if possible. Secondary, start with the primary assessment: After head trauma, victims must be assessed for life-threatening injury. The MARCH (massive hemorrhage, airway, respiration, circulation, hypo-/hyperthermia, hike/heli) should be assessed. MARCH is used instead of the of the standard ABCDE, since it’s more applicable to the wilderness setting. Nevertheless, ATLS-guidelines should be taken into account. If cervical spine injury, skull fracture or moderate/severe brain injury is suspected, the patient should be stabilized and evacuated immediately according to the Wilderness Medical Society guidelines for spine immobilization. The survival and outcome of severe head injury in the wilderness correlate directly with the rapidity of evacuation. High-risk group patients include a Glasgow Coma Scale (GCS) of ≤13, focal neurologic signs, repetitive vomiting, and posttraumatic seizures. Generally speaking, every indication for a CT in a regular EM-practice, is an indication for rapid evacuation. Henceforth, the Canadian CT Head Rule calculator can be used. After the primary assessment and initial management, patients should receive an (S)AMPLE history and head to toe secondary survey.
Second Survey & ongoing survey
The goal of the secondary survey is to identify and treat any remaining less-critical injuries and illnesses. An abbreviated medical history should be performed (SAMPLE) and head-to-toe physical examination. This should never be a reason to delay evacuation. The acronym SAMPLE can be useful to assess a patient’s history. For head-trauma:
Signs & Symptoms: check the pupils, abnormal posturing, respiratory depression, and the Cushing triad: hypertension, bradycardia, and irregular respiration. Also, check for a Battle sign and raccoon eyes (basal skull fracture).
Allergies: no special notice.
Medicines: inform about prescribed drugs, especially those interacting with blood clotting.
Past: pre-existent neurological status, other diseases.
Last meal: to assess the risk of aspiration.
Event: what happened exactly? How did you fall?
The neurologic status of a patient can deteriorate rapidly in case of head trauma. Therefore, the vitals, GCS, and physical examination should be assessed and repeated regularly.
Pathophysiology
Traumatic Brain Injury can be classified according to the pathophysiology:
Primary brain injury: The immediate and permanent damage to brain tissue by the traumatic event. Injuries can be focal: Hematomas, contusions, and lacerations, or diffuse: Axonal shearing and concussion.
The response to the initial mechanical trauma can cause secondary brain injury. This may exacerbate the effects of the primary trauma, e.g., increased intracranial pressure, hypoxia, hypotension, hypothermia, hyponatremia, hypo- and hyperglycemia, edema, and also increased liberation of mediators, toxic amino acids, proteolytic enzymes, or oxygen radicals. Secondary brain injuries are potentially preventable and reversible.
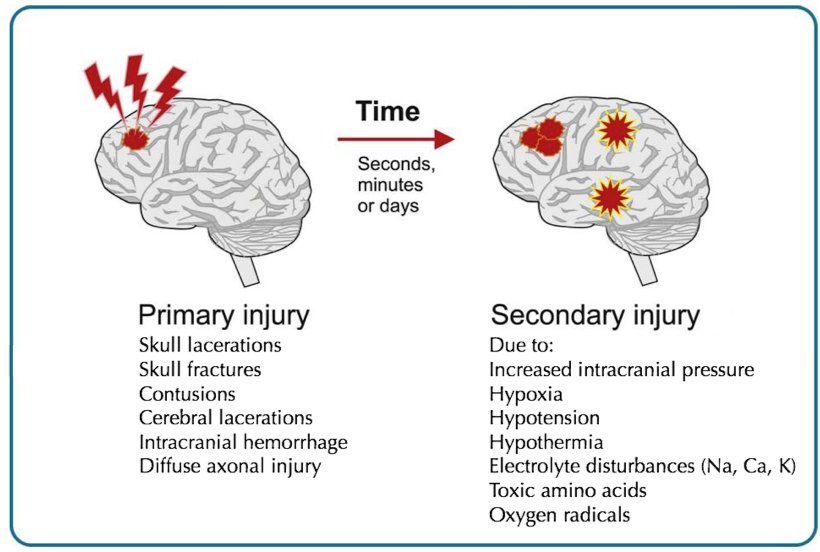
To prevent secondary injury, edema should be prevented, but the Mean Arterial Pressure (MAP) should be sufficient for brain perfusion. The Cerebral Perfusion Pressure (CCP) depends on the MAP and intracranial pressure (ICP). In a formula, CCP=MAP-ICP. Therefore, the ICP should be reduced (mannitol, 0.9% saline) and hypotension should not be accepted (fluids, vasopressors).
Conclusion
Head-injuries account for a worldwide burden and certain athletes are at increased risk. Patients with a mild/severe head injury should be stabilized and evacuated immediately. Acquaint yourself with medevac procedures, in case of possibly severe trauma in an austere environment. Mild/minor injuries and concussion management will be discussed next week.
Literature:
- Concussion Management in the Wilderness – Wright et al., Wilderness & Environmental Medicine (2014)
- Auerbach’s Wilderness Medicine ““ Wilderness trauma, surgical emergencies, and wound management, section on head injury




