I remember well when Joost Hopman, a medical microbiologist at Radboud UMC, lectured on an Outdoor Medicine day about parasites. With tremendous fascination and admiration for nature, he presented “phenomenal parasites” that target us. These professional parasites inhabit our bodies. In this process, they seriously damage our organs, leave the body like a house party that has gotten out of hand, and cause the host a lot of misery. Even worse, it can take some time before you realize a party is going on. Especially around the tropics, parasitic infections cause a considerable disease burden. What parasites can you encounter there and what should you look out for? We present a top four:
Filariasis
Filariasis is a parasitic worm infection transmitted by mosquitoes around the tropics and sub-tropics. These worms block lymphatic drainage, causing severe lymphedema, known as elephantiasis (popularly known as elephantiasis). This can be accompanied by fever, lymphangitis, and complications such as pulmonary eosinophilia. Filariasis mainly affects the local population, 120 million people worldwide, and is listed as a Neglected Tropical Disease (NTD). Short-term tropical visits give a low risk of infection. Prevention consists of mosquito-repellent measures. The parasites can be detected microscopically or serologically in the blood and treatment is done with diethylcarbamazine, ivermectin (for concurrent onchocerciasis infection), or doxycycline.

Helminthiasis
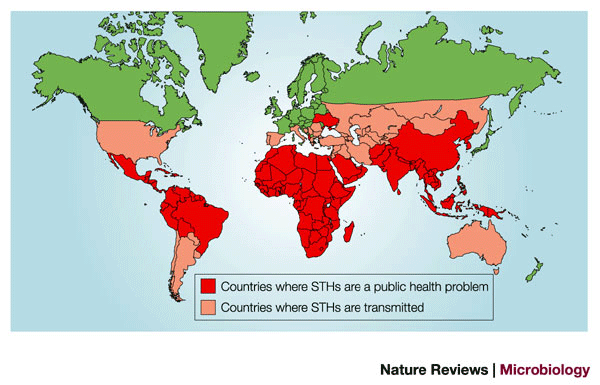
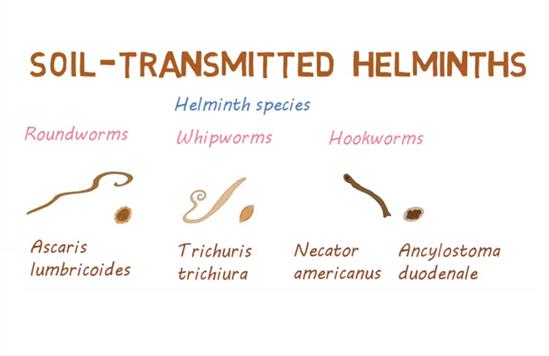
Helminthiasis is an infection with a worm (helminth). Notorious worms are the roundworm (Ascaris lumbricoides), whipworm (Trichuris trichiura), and hookworm (Ancylostoma duodenale, Necator americanus, and Strongyloides stercoralis), bundled together under the name “soil-transmitted helminths” in that they can be transmitted through contaminated soil. These parasites are also listed as Neglected Tropical Diseases (NTD), with an estimated 2 billion infected worldwide. The eggs of these parasites are passed through feces (Ascaris & whipworm). The hookworm can also invade the skin directly, such as from contact with bare feet. The risk of infection for travelers is quite small. Symptoms occur particularly in children and consist of anemia and protein deficiency due to gastrointestinal blood loss. Nevertheless, very unpleasant (late) complications can also occur especially in immunocompromised patients, such as secondary E. coli meningitis. The diagnosis of worm infections relies on the detection of eggs, larvae, or the adult worm in feces, blood, or tissue and is suspected by eosinophilia. Treatment is with antihelminthics. In addition to the above three worms, there are numerous other worm infections that can cause problems.
Malaria
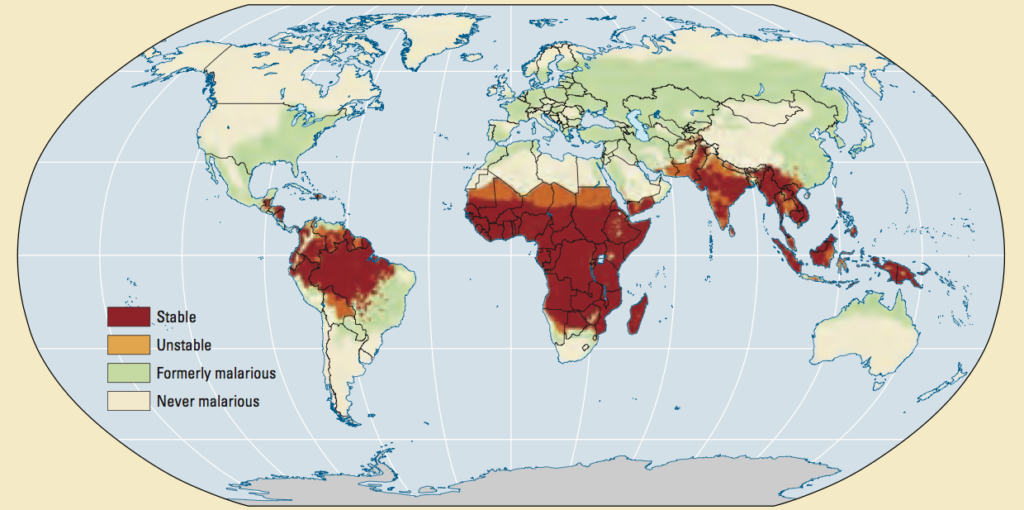
Of course, malaria should not be missing from this list. Although named after the Italian mala aria, which means ‘bad air’ – denoted to the unwholesome atmosphere caused by the exhalations of marshes, to which the disease was formerly attributed – malaria is caused by parasites and transmitted through mosquitoes. Particularly in sub-Saharan Africa, there is a huge disease burden from malaria, with an estimated 620,000 deaths per year, although there has already been a huge decline due to efforts by the WHO and similar organizations. The severity of the disease is strongly related to the type of parasite. Symptoms that are prominent are fever, headache, and chills, but can be nonspecific. In the Netherlands, 200-300 patients are diagnosed with imported malaria each year. Diagnosis consists of a blood smear and thick-drop microscopy. Treatment consists of artemisinin-based combination therapy (ACT) or chloroquine as an alternative. Severe forms are treated with intravenous artesunate in combination with ACT. Prevention consists of chemoprophylaxis, protective clothing, DEET, and mosquito nets.
Schistosomiasis
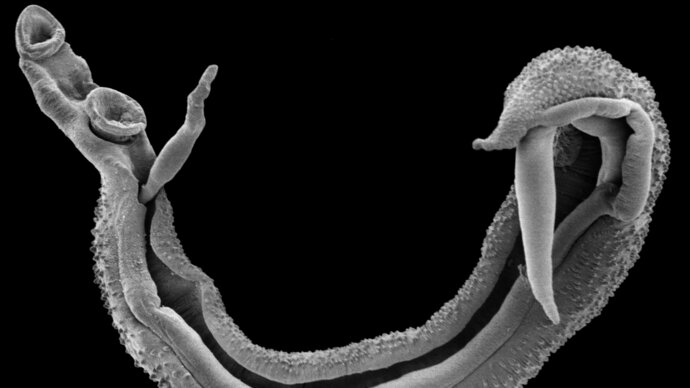
Schistosomiasis is relatively unknown to laymen, although along with malaria, the disease burden dominates the global parasitic top. Schistosomiasis is caused by parasitic worms and is also known as Bilharzia. These worms live in freshwater snails and can enter the skin through contact with contaminated fresh water. Penetration of these worms into the skin can cause a swimmer’s itch (cercarial dermatitis). Furthermore, an acute infection may be accompanied by Katayama fever with similar symptoms that may resemble malaria or influenza, but acute infection is usually asymptomatic. One to two months later, the body develops an inflammatory response against the eggs of the worms somewhere in the body, for example, the bladder, small intestine, or other organs, which may be accompanied by fever, chills, cough, and muscle pain, depending on the type of parasite (Mansoni, Haematobium or other variants). The diagnosis is made microscopically in urine or fecal samples, or serologically. The treatment is with praziquantel.
In addition to the above, there are many other parasites and other infections to be wary of in the (sub) tropics. Adequate preparation with preventative measures, vaccinations, and travel advice can drastically reduce the risk of infection. Would you like to learn more about infectious diseases, gain skills in the pre-hospital jungle setting and know what to do in case of a snake bite? Then check out our jungle medicine course.




