In 2015, drowning accounted for at least 360.000 deaths worldwide. It is the third leading cause of unintentional injury death worldwide, accounting for 7% of all injury-related deaths. Most of the incidents occur in low or middle-income countries. With the summertime being present, people tend to swim more often and submersion or drowning happens more often in Europe. This short article intends to give a brief summary on how to prevent a person from drowning and, how to recognize and treat a person who has submerged or drowned.
Definition
Drowning has most recently been defined as “the process of experiencing respiratory impairment from submersion/immersion in liquid“. Outcomes of drowning should be classified as death, morbidity, and no morbidity. Recent guidelines suggest that the term “submersion injury” or non-fatal drowning should replace “near-drowning”, although the latter is still commonly used. Although previously thought to be of physiologic relevance (salt vs fresh water, wet vs dry), years of data related to human drowning pathophysiology show that these are not valid distinctions, because the final common pathway is hypoxemia and eventually cardiopulmonary arrest.
Dry drowning
With so-called dry drowning, a term commonly used in the non-medical environment, by Laymen’s terms, is the result of drowning without water entering/reaching the lungs. Instead, breathing underwater causes the vocal cords to spasm and close up. That shuts off the airways, making it hard to breathe. The signs are similar to drowning. Frequently it is not possible to determine at the scene whether or not water was aspirated, particularly when the amount of water is small. In summary: the term “dry drowning” however is needlessly ambiguous. It should be avoided!
Shallow Water Blackout
A special cause of drowning that occurs in people who hyperventilate before entering the water for an underwater swim. The hyperventilation significantly reduces PaCO2 without increasing oxygen storage. The vigorous underwater activity uses the available oxygen, causing hypoxemia, but before sufficient CO2 accumulates to provide a stimulus to return to the surface. The patient loses consciousness due to the hypoxemia and drowns.
Pathophysiology of drowning
When a drowning person can no longer keep his or her airway clear, water entering the mouth is voluntarily spat out or swallowed. The next conscious response is to hold one’s breath, but this lasts for no more than about a minute. When the inspiratory drive is too high to resist, some amount of water is aspirated into the airways, and coughing occurs as a reflex response. Sometimes laryngospasm occurs, but in such cases, it is rapidly terminated by the onset of brain hypoxia. If the person is not rescued, aspiration of water continues, and hypoxemia quickly leads to loss of consciousness and apnoea. The sequence of cardiac-rhythm deterioration is usually tachycardia followed by bradycardia, pulseless electrical activity, and, finally, asystole. The whole drowning process, from submersion or immersion to cardiac arrest, usually occurs in seconds to a few minutes, but in unusual situations, such as hypothermia or drowning in ice water, this process can last for an hour.
If the person is rescued alive, the clinical picture is determined predominantly by the amount of water that has been aspirated and its effects. Water in the alveoli causes surfactant dysfunction and washout. Aspiration of salt- or fresh water cause similar degrees of injury, although with differences in osmotic gradients. In either situation, the effect of the osmotic gradient on the very delicate alveolar”“capillary membrane disrupts the integrity of the membrane, increases its permeability, and exacerbates fluid, plasma, and electrolyte shifts. The clinical picture of the damage caused to the alveolar”“capillary membrane is a massive, often bloodstained, pulmonary edema that decreases the exchange of oxygen and carbon dioxide. The combined effects of fluids in the lungs, loss of surfactant, and increased permeability of the alveolar”“capillary membrane result in decreased lung compliance, increased regions of very low or zero (or decreased) ventilation to perfusion ratio in the lungs, atelectasis, and bronchospasm.
If cardiopulmonary resuscitation (CPR) is required, the risk of neurologic damage is similar to that in other instances of cardiac arrest. However, hypothermia associated with drowning can provide a protective mechanism that allows persons to survive prolonged submersion episodes.Hypothermia can reduce the consumption of oxygen in the brain, delaying cellular anoxia and ATP depletion. Hypothermia reduces the electrical and metabolic activity of the brain in a temperature-dependent fashion. The rate of cerebral oxygen consumption is reduced by approximately 5% for each reduction of 1°C in temperature within the range of 37°C to 20°C.

Risk factors
Key risk factors for drowning are male sex, an age fewer than 14 years, alcohol use, low income, poor education, rural residency, aquatic exposure, risky behavior, and lack of supervision. For people with epilepsy, the risk of drowning is 15 to 19 times as high as the risk for those who do not have epilepsy.
How to prevent drowning?
Prevention of drowning focusses mainly on the risk factors mentioned above, in summary: it is based on being cautious and rational at all times when there’s water involved.
Children are at risk of drowning, so teaching them how to swim is a good start, but swimming lessons alone do not make a child “drowning proof”. In a drowning situation, children may not have the body strength, judgment, or emotional reserve to allow self-rescue.
More than 50% of adult drowning-deaths are believed to be alcohol-related. Know your limits. Feats of endurance and demonstrations of bravado in dangerous rapids or surf are for idiots. This is the main difference in the incidence of drowning accidents being twice as high in male patients rather than in female patients.
How to recognize a person drowning?
A person who is drowning may be obviously struggling, but sometimes it takes an astute observer to recognize that a person in the water is in trouble, because the victim may not be strong or alert enough to call or signal for help. Less obvious indications of drowning include (what does drowning look like?):
• Bobbing up and down in the water with wide open mouth and rapid or gasping breaths.
• Head tilted back in the water with open mouth.
• Mouth at or below water level.
• Eyes “glassy” or closed; blank stare.
• Eyes and forehead covered with hair.
• Not using the legs at all to swim or remain afloat while remaining upright in the water.
• Purposeless swimming.
• Swimming hard without forwarding progress.
• Within earshot but not responding to your call for a response.
• Children who are quiet in the water.
Note: contrary to popular perception, nearly half of drowning cases occur in inland waterways: drowning in a swimming pool is relatively rare.
A Dutch university is currently programming a drone to recognise drowning victims, might this be the future? Note: contrary to popular perception, nearly half of drowning cases occur in inland waterways: drowning in a swimming pool is relatively rare.
Basic life support of a drowning victim.
If you anticipate that you might need to rescue a drowning person, you should know how to swim (see this rescue swimming video), complete an in-water rescue, start rescue breathing and CPR, and summon help.
1. Remove the victim from the water. In-water resuscitation is difficult at best. It should be attempted only by a trained rescuer. Administering a couple of rescue breaths to a nonbreathing victim while he or she is still in the water may be helpful.
2. After the victim is removed from the water, check for breathing. Open the mouth and sweep it clean with two fingers. Align the victim on the ground with his head at the level of his trunk (not head down). Begin mouth-to-mouth or mouth”“to”“mouth-and-nose (for a child) breathing, if necessary. Administer 5 initial rescue breaths.
3. Check for pulses and begin chest compressions if necessary. For drowning, use the “ABC” (airway, breathing, circulation/chest compressions) order for CPR.
4. If the victim is unconscious but breathing, place him in the lateral lying rescue position with the head higher than the trunk.
5. Administer oxygen at a flow rate of 15 liters per minute by non-rebreathing face mask.
6. Suspect a broken neck in the appropriate circumstances. Don’t delay resuscitation procedures in an attempt to address possible spinal injuries.
7. The Heimlich maneuver and other choking protocols (e.g., back slaps, chest hugs) are not recommended for use in the rescue of drowning victims
8. Hypothermia is commonly associated with drowning. Cover the victim above and below with blankets and remove all wet clothing. Remember, “no one is dead until he is warm and dead.”
9. If the victim responds to your measures, the following guidelines for further medical assistance are recommended:
Persons who require further evaluation/assistance (likely at a hospital): Loss of consciousness (even if briefly) at any point; received rescue breathing; underwent CPR; serious condition (e.g., heart attack, spinal or other significant injury, asthma, marine animal sting, intoxication, altered mental status) suspected. A person who is already short of breath and coughing may deteriorate quickly.
Persons who may be considered to be safely released from care at the scene: Victim should be observed for 15 minutes and seen to have all of the following: no coughing, normal rate of breathing, normal pulse (strength and rate), normal skin color and temperature, no shivering, fully awake and alert. These victims will nearly always do well. However, it should be noted that on occasion a person who has suffered a drowning event and appears well at first may develop a cough, shortness of breath, or fever. If this happens, they should be brought promptly to medical attention.
Advanced Life support:
In addition to providing immediate basic life support, it is important to alert advanced-life-support teams as soon as possible. Because of the wide variety of clinical presentations of drowning, a classification system of six grades, with higher numbers indicating more severe impairment, can help to stratify risk and guide interventions.
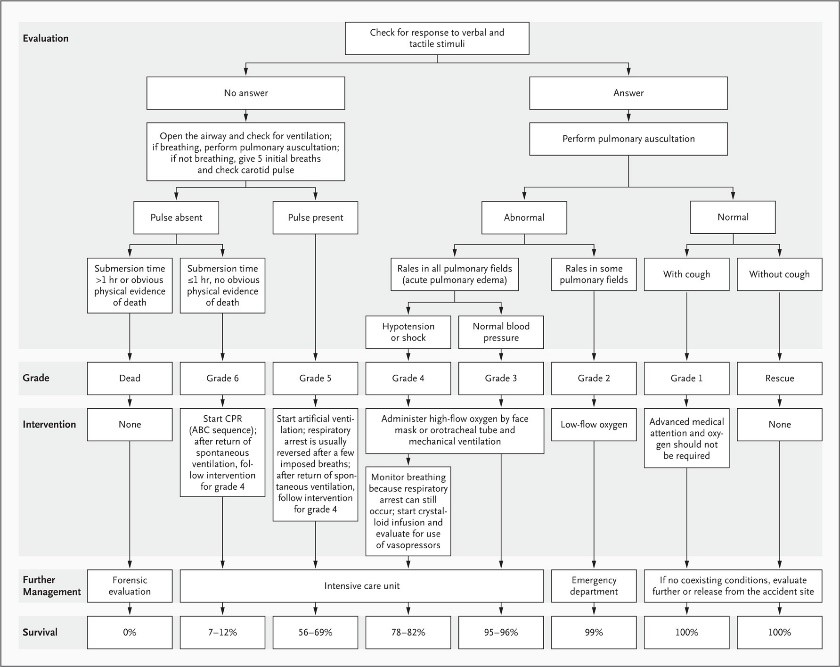
A person with pulmonary damage may initially be able to maintain adequate oxygenation through an abnormally high respiratory rate and can be treated by the administration of oxygen by face mask at a rate of 15 liters of oxygen per minute. Early intubation and mechanical ventilation are indicated when the person shows signs of deterioration or fatigue (grade 3 or 4). Once intubated, most persons can be oxygenated and ventilated effectively. Although copious pulmonary-edema fluid may appear in the endotracheal tube, suctioning can disturb oxygenation and should be balanced against the need to ventilate and oxygenate. Providers of prehospital care should ensure that there is adequate oxygenation to maintain arterial saturation between 92% and 96%, while also ensuring adequate chest rise during ventilation. Ventilation with positive end-expiratory pressure should be initiated as soon as possible to increase oxygenation.
Peripheral venous access is the preferred route for drug administration in the prehospital setting. Intraosseous access is an alternative route. Endotracheal administration of drugs is not recommended. If hypotension is not corrected by oxygenation, a rapid crystalloid infusion should be administered, regardless of whether salt water or fresh water has been inhaled.
The presenting rhythm in cases of cardiac arrest after drowning (grade 6) is usually asystole or pulseless electrical activity. Ventricular fibrillation is rarely reported but may occur if there is a history of coronary artery disease or in the presence of severe hypothermia. During CPR, if ventilation and chest compression do not result in cardiac activity, a series of intravenous doses of norepinephrine or epinephrine, at an individual dose of 1 mg (or 0.01 mg per kilogram of body weight) can be considered. Because of the mechanisms of cardiac arrest due to hypoxia and the effects of hypothermia, a higher subsequent dose, although controversial, may be considered if the initial doses are ineffective.
Use of AED in Cases of Drowning
The cost-effectiveness of providing an automated external defibrillator (AED) at sites of aquatic activity has been debated. The predominant cardiac-arrest rhythm in drowning is asystole. Of course, cardiac arrests at aquatic sites occur from causes other than drowning, and the availability of an AED may be lifesaving.
Summary
• The basic pathophysiology of submersion injury is respiratory failure with hypoxemia and resultant cardiac ischemia and neurologic injury.
• Children are at risk of submersion injuries and it mostly happens in third world countries.
• A person drowning can be very hard to recognize, while the symptoms differ and the process of drowning can occur very fast.
• The treatment is aimed to immediate and aggressive initiation of ventilation and oxygenation (BLS should start with 5 rescue breaths).
• If pulmonary auscultation is abnormal, patients should be admitted to an emergency department.
Additional information
Interested and willing to improve your knowledge about this subject and more subjects alike? Join the Dive & Marine life support course! It will take place from 15-09-2018 until 22-09-2018 on Bonaire Island!

References
1 Organisation WH. Drowning Fact Sheat. http://wwwwhoint/en/news-room/fact-sheets/detail/drowning. 15 January 2018.
2 Handley AJ. Drowning. BMJ (Clinical research ed). 2014;348:g1734.
3 Warrell DA, Cox TM, Firth JD. Oxford Textbook of Medicine.
4 Chris Johnson SA, Jon Dallimore, Chris Imray, Shane Winser, James Moore, David Warrel. Oxford Handbook Of Expedition And Wilderness Medicine. April 2015(Second edition).
5 Szpilman D, Bierens JJ, Handley AJ, Orlowski JP. Drowning. The New England journal of medicine. 2012;366(22):2102-10.
6 Dipak Chandy MLW, MD, Daniel F Danzl, MD, Jonathan Grayzel, MD, FAAEM. Drowning (submersion injuries). Up to date. Literature review current through: May 2018. | This topic last updated: Dec 11, 2017.
7 Paul S. Auerback M. Medicine for the outdoors.6th edition.1. Paul S. Auerback M. Medicine for the outdoors.6th edition.
This was the first article I wrote for Outdoor Medicine, comments or feedback? I’d like to hear from you. [email protected]




