With the background information of the previous article taken into account, now the 3 best known altitude-related disorders will be discussed. It is important to realize that this concerns a range of disorders, which can occur either individually or at the same time, and can also shade off into one another.

Acute Mountain Sickness; AMS
Acute altitude sickness has a whole range of symptoms, from mild to very severe. There are several theories about the etiology of AMS, but one of them is that it is a mild type of altitude cerebral edema (HACE). Generally the symptoms arise within 6-24 hours after reaching an altitude above 2500 m and disappear within a day if the patient stays at the same altitude. It is important to realize that after every ascent to a new altitude, the body needs to acclimatize again; therefore, after every ascent there is a risk of altitude sickness.
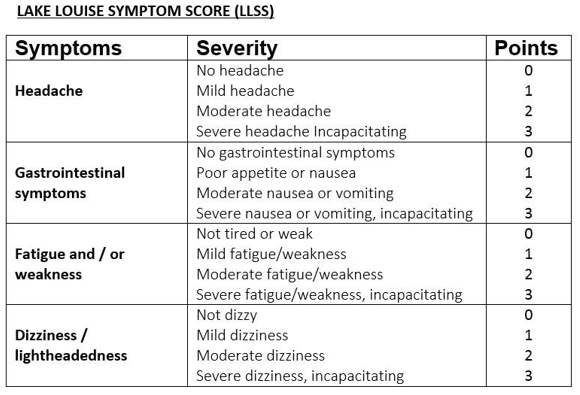
AMS is diagnosed using the Lake Louise AMS-score list (see image). Points are scored on the following symptoms: (throbbing) headaches, loss of appetite/nausea/vomiting, fatigue/weakness and dizziness. A score of three or more means AMS.
In altitude sickness, the patient’s level of consciousness is therefore not reduced.
High Altitude Cerebral Edema; HACE
HACE is often preceded by AMS. It is a life-threatening condition if not adequately treated. In the case of HACE there is edema in the brain, caused by the following presumed mechanisms; reduced cerebral autoregulation, capillary leakage as a result of a hypoxia-induced inflammatory reaction of the vascular walls and swelling of the brain cells. The effect is swelling of the brain and thus increased intracranial pressure. The core symptoms that result from this are ataxia, severe headache and an altered state of consciousness.
Symptoms that may also occur include severe nausea and vomiting and behavioral changes; the patient may behave aggressively or show behaviour that does not otherwise suit him.

High Altitude Pulmonary Edema; HAPE
HAPE is the least common altitude-related disorder. However, this potentially deadly disease is really dangerous because it can develop without being preceded by symptoms of acute altitude sickness, which may serve as warning signs. Usually this disease develops in 2-5 days after being exposed to a new altitude, but it can also develop within a few hours.
In the case of HAPE, there is acummulation of fluid in the lungs. The underlying pathophysiology is, as described earlier, increased pulmonary arterial blood pressure by hypoxic pulmonary vasoconstriction. This is a normal physiological reaction when being exposed to altitude, but some people develop an above average increase in pulmonary arterial blood pressure. Due to this increased pressure and flow, endothelial damage occurs, causing edema.
The main symptom is shortness of breath; there is an oxygen desaturation that is not proportional to the physical effort. There is tachycardia as well. Often there is also a dry cough and a productive cough with pink, frothy sputum at a later stage. The patient cannot lie flat.

For a brief overview of the symptoms and treatment of AMS, HACE and HAPE, check the lecture of the University of California Television of Emergency Medicine of doctor Chriss Colwell
General non-drug treatment of altitude-related disorders
The most important of all is descending, even at night or in bad weather. Only in case of a mild form of AMS, the patient can stay at the same altitude and take rest to give the body the time it needs to acclimatize.
Rest is the second important advice; even if there is only a mild form of altitude sickness. Especially in the case of HACE/HAPE, even the smallest effort can worsen the symptoms. In HACE/HAPE, patients should be carried down, or, if this is not possible, they should get rid of their backpacks and should be supported while walking. Patients with moderate/severe AMS are usually still able to walk down by themselves.
In the case of HACE/HAPE, oxygen or hyperbaric therapy (as with the Gamow bag) can be lifesaving. It will stabilise the patient’s condition during or before the descent, especially if descending is not immediately possible due to dangerous terrain or not enough porters.
Always ensure that the patient stays warm and well hydrated.

Drug treatment
In the case of AMS, acetazolamide (DIAMOX) can be used. The mechanism of action of acetazolamide is multifactorially determined and not fully understood, but one of the effects is that it has a diuretic effect and increases renal sodium and bicarbonate excretion. Overall, it increases the respiratory rate and thus speeds up the acclimatization process. The prophylactic dosage for altitude sickness is 125 mg twice a day; the therapeutic dosage is 250 mg twice a day for as long as the patient stays at altitude.
Dexamethasone is an effective treatment of HACE. It can be administered orally, intramuscularly or intravenously. The initial dosage is 8 mg, followed by 4 mg four times a day for as long as the patient stays at altitude.
In the case of HAPE, the calcium antagonist nifedipine can be used, whether or not in combination with oxygen (depending on availability). It is important to realize that it has an antihypertensive effect; especially the combination with dehydratrion will put the patient at greater risk of hypotension. The dosage is 30 mg twice a day.
For more information about drug use in altitude-related disorders, check this article: Drug Use and Misuse in the Mountains: A UIAA MedCom Consensus Guide for Medical Professionals.

Literature
Diercks, R. (2016). Leerboek sportgeneeskunde (1e editie). Houten, Nederland: Bohn Stafleu van Loghum.
Donegani, E., Paal, P., …, & Hillebrandt, D. (2016). Drug Use and Misuse in the Mountains: a UIAA MedCom Consensus Guide for Medical Professionals. High alt med biol 17(3).
Duff, J. (2007). First aid and wilderness medicine (10e editie). Milnthorpe, UK: Cicerone Press
Johnson, C., Anderson, …, & Warrel, D. (2008). Oxford handbook of expedition and wilderness medicine (2e editie). Oxford, UK: Oxford University Press
Roach, R.C., Hackett, P.H., …, & Baillie, J.K. (2018). The 2018 Lake Louise Acute Mountain Sickness Score. High alt med biol 19(1).
Willems, H. (2014). Hoogteziekte, theorie en praktijk (1e editie). Huis ter Heide, Nederland: Han Willems.
The UIAA guideline: https://www.theuiaa.org/mountain-medicine/medical-advice/
The WMS guideline: https://www.wemjournal.org/article/S1080-6032(14)00257-9/fulltext




