Last week, we ran over the evaluation of severy head injury, briefly summarized in the figure below (MARCH). Nonetheless, there’s still some work to be done when the need for a CT-scan, and therefore rapid evacuation, is ruled out.
Evaluation of non-severe head injury
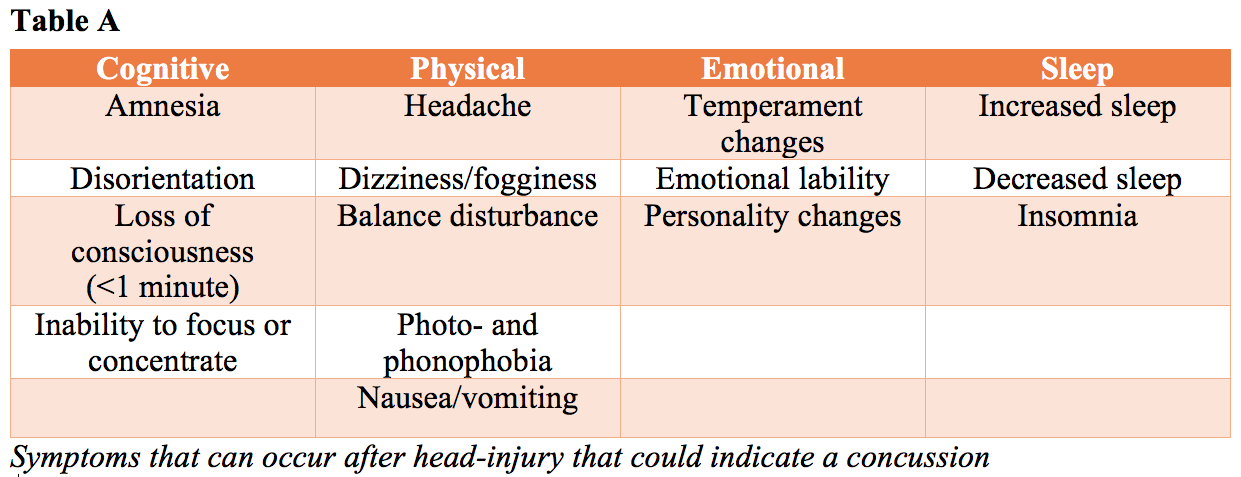
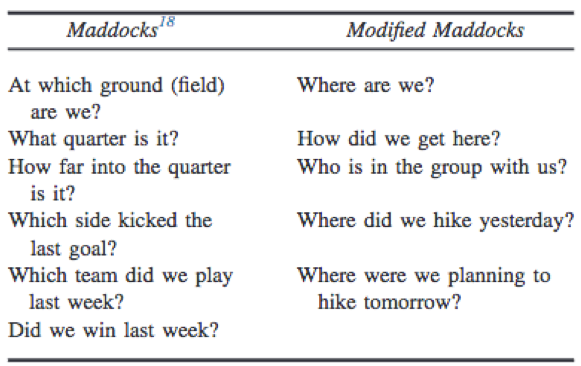
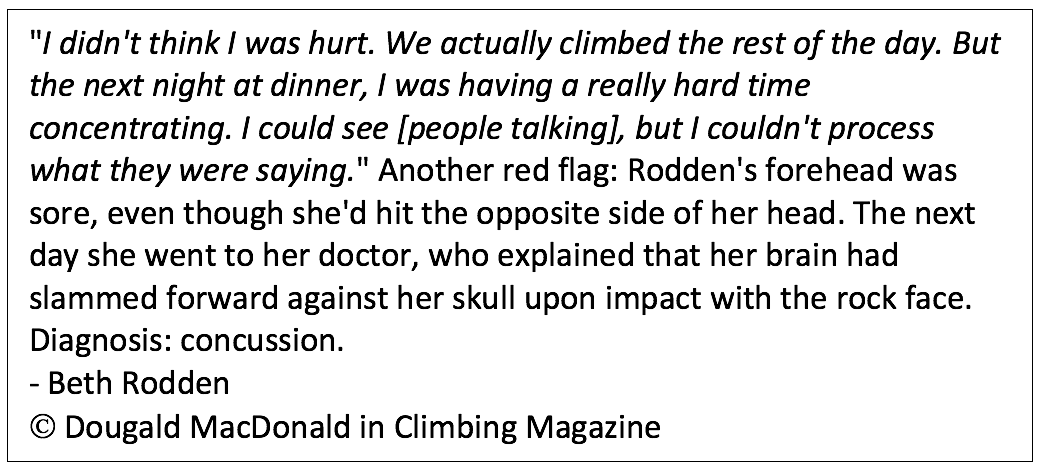
Several concussion tools are available, like the SCAT5. However, at present, there is no perfect diagnostic test or marker that clinicians can rely on for immediate diagnosis of concussion in the sporting environment, and frequently used tools may not practical for a wilderness setting. Symptoms that may indicate a concussion are summarized in table A. These could appear even some hours or days after trauma. The modified Maddocks as shown below can be used. Furthermore, physical examination/secondary survey should be performed, focusing on the neurological status, balance, cranial nerves, and short-term memory.
Differential Diagnosis
Traumatic head injury can be an evident cause of symptoms. However, diagnosing and managing a concussion can be challenging, as signs and symptoms could be vague, delayed, and difficult to interpret. In fact, according to the 5th International Conference on Concussion in Sport in 2016, “Concussion is considered to be among the most complex injuries in sports medicine to diagnose, assess, and manage“. Keep in mind that an altered mental state has a broad variety of underlying causes which should be taken into account as well, including but not limited to Acute Mountain Sickness (AMS), High Altitude Cerebral Edema (HACE), dehydration, exercise-associated hyponatremia (EAH), intoxications, poisoning, or sleep deprivation.
Management of concussions and minor/mild brain injury
Improperly managed concussions can lead to prolonged physical and physiological symptoms, while patients with properly managed concussions are able to recover completely without long-term sequelae. Key is absolute rest from physical and mental stimulation followed by gradual return to activity in steps, once symptoms resolve. Athletes with more severe symptoms initially, or a past medical history of multiple concussions, often require longer recovery times. For those injuries that occur two or more days of travel from a base and medical attention, the patient either should rest until symptoms improve before moving on, or evacuation should be reconsidered. If symptoms return during any period of exertion, the individual must rest 24 hours. Once back in a controlled or urban setting, patients should be restricted from mentally stimulating activities, including reading, video games, and text messaging.
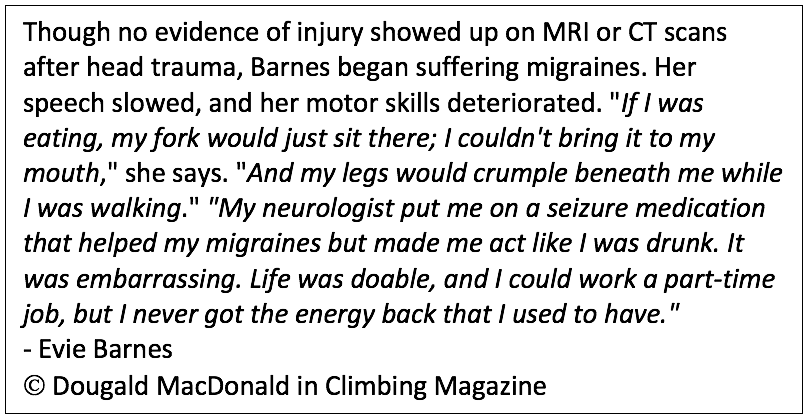
Post-concussion syndrome
Post-concussion syndrome is a complex disorder in which various symptoms “” such as headaches and dizziness “” last for weeks, sometimes months and even years after the injury that caused the concussion. In most people, symptoms occur within the first seven to ten days and go away within three months. More research is still needed to better understand how and why post-concussion syndrome happens after some injuries and not others. The same applies to repetitive head trauma, another entity. These injuries have gained more attention over the last couple of years since it’s possibly linked to chronic traumatic encephalopathy (TED-talk). Research of former football players led to a body of evidence questioning the impact of contact sports on the brain, featured in the movie: Concussion (2015).
Rehabilitation
About 60% of adults with moderate head injuries and 85% with severe head injury remain disabled one year after the accident. As mentioned before, concussions often resolve within 10 days of injury. Those athletes who show a slow recovery (>10 days) should be managed with a multidisciplinary team of health care professional with experience and expertise in sports-related concussion. Cervicovestibular rehabilitation should be considered since it reduces the time to return to sport. Although the use of helmets may not stop a concussion, it may reduce the severity of one, which is of great importance in (extreme) sports. Non-helmet-wearers are more than twice as likely to suffer a severe head injury than helmet wearers in climbing and other sports. (British Mountaineering Council, 2007).

Conclusion
Head-injuries account for a worldwide burden and certain athletes are at increased risk. Patients with mild/severe head injury should be stabilized and evacuated immediately. Acquaint yourself with medevac procedures, in case of possibly severe trauma in an austere environment. Minor head injuries and concussion management can be daunting for both the medical professional and the athlete. The key to complete recovery is absolute rest with stepwise reactivation.
Concussions – Eric A. Weiss. ‘Wilderness & Travel Medicine’
Concussion Management in the Wilderness – Wright et al., Wilderness & Environmental Medicine (2014)
Auerbach’s Wilderness Medicine ““ Wilderness trauma, surgical emergencies, and wound management, section on head injury
No-Brainer? Why Do So Many Climbers Not Wear Helmets? – Dougald MacDonald, Climbing Magazine, Jul 30, 2013.
Extreme Sports Medicine: Rehabilitation of Extreme Sports Injuries, Maggie Henjum, Carly Mattson, and Francesco Feletti





