Half of March, Annemarie Wuister finished her General Practice training. Ready to start her career as a locum GP. She had it all figured out: a locum job in homeport the Hague, whereafter she would go to Aruba to work at a general practice and enjoy kitesurfing in her free time. Right at the time of her graduation, the government starts taking serious measures to control the pandemic. Aruba is a no-go. Thereby, consultations in general practice decrease dramatically, resulting in less locum work.
Nevertheless, she didn’t feel like sitting this crisis out when the world was on fire. Besides, this wasn’t the first epidemic she encountered. She performed research during the Q-fever epidemics, worked in the intensive care unit during the flue-epidemic of winter 2015, and worked in the refugee camps of Lesbos and Samos (shock en trauma op Lesbos). Furthermore, she realizes that it is essential to have a flexible attitude during these times of crises.
For this reason, she starts to work on special COVID-stations. These places are organized to see first-line COVID-suspected patients. Personal protective equipment (PPE) can be saved this way, and contamination between patients is mitigated. Despite the work on these stations, she isn’t able to fill all the gaps as a freelancer. Thinking back to her days on the Intensive Care, she sends her old employer, intensivist Koeman in Haga hospital an e-mail if she can be of any use. Contrary to her expectations, they apply positively. They were short of experienced doctors. 18 Intensive Care Unit (ICU)-beds were scaled up to 28, of which 24 were being used for COVID-patients. Before realizing it, a just-finished GP was dressed in a white cloak again, next to a ventilation machine: a unique and overwhelming experience.
She had to shift some mental gears. “As a general practitioner, I establish a connection with my patients. I’m open to their feelings and trained to empathize. On the ICU-ward, nearly all patients are being ventilated, so communicating and making contact with patients is impossible. Also, it’s quite intense, it can be life-saving, but some cases are very dreadful, and outcomes can change unexpectedly.
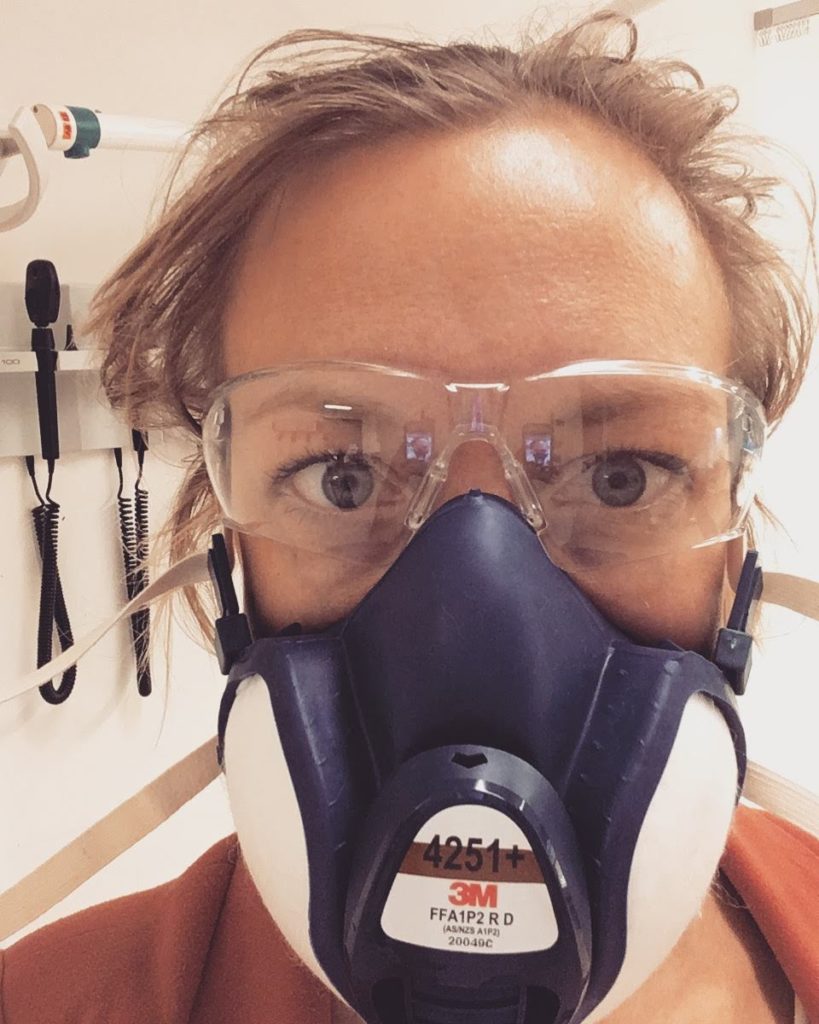
Visitors weren’t allowed during the beginning of the crisis due to a shortage of personal protective equipment (PPE). Also, personal belongings like photographs and get-well cards weren’t allowed in the room because of the risk of contamination. Normally, face-to-face contact with the family and relatives helped to familiarize and humanize with the patients. With telecommunication only, it’s different, and it makes this aspect much harder. The patients’ appearance changes a lot. As a result of fluid, the faces get swollen and facial characteristics to seem to disappear. Before the crisis, photos helped to picture the faces before the critical illness. One of the toughest moments she remembers was when a patient was nearly passing away and the family was allowed to say a final goodbye. As a result of weeks of mechanical ventilation, the family didn’t recognize their own loved one and didn’t dare to come close.
”To family members, it’s nearly impossible to explain what critical illness is and what it does to the body of the patient.” As result family members don’t seem to understand the severity of the illness or a poor prognosis. She notices as well, that hospitalization on the ICU and cases of resuscitation are sometimes taken too lightly in general practice. These treatments are tough, long, with disputable outcomes and should be considered carefully. “It’s a good thing this crisis focuses the attention also to the quality of life, the rehabilitation period after hospitalization, and adverse outcomes like psychological trauma after long, intensive treatment.”
The shift between Intensive Care ward and COVID-posts was quite pleasant. Despite covering the same disease, the presenting symptoms are, needless to say, very different. On the Intensive Care ward, it seemed everybody had a very poor prognosis. At the same time, she observed people recovering at home. After weeks of seeing patients pass away after a long and demanding treatment on the Intensive Care, it seemed like even the intensivists lost some hope. Fortunately, she already noticed the decline of hospitalization of COVID-positive patients.
She wasn’t apprehensive for COVID herself: “I hope I already had an asymptomatic infection”. On the other hand, she feels uncertainty as a freelancer. “A period without work and therefore, no income could be quite challenging when she would become ill herself.
Meanwhile, the COVID-patients on intensive care has been decreased to normal numbers. She still does some shifts on the COVID-posts, but those are being reduced as well. The new challenge is how to organize and scale healthcare in a safe way after the first wave of this pandemic. “Flexibility during this crisis appears to be an important skill” – according to Annemarie Wuister.




